 or click Activities, Insurance Billing, Do Billing. The billing screen will load.
or click Activities, Insurance Billing, Do Billing. The billing screen will load.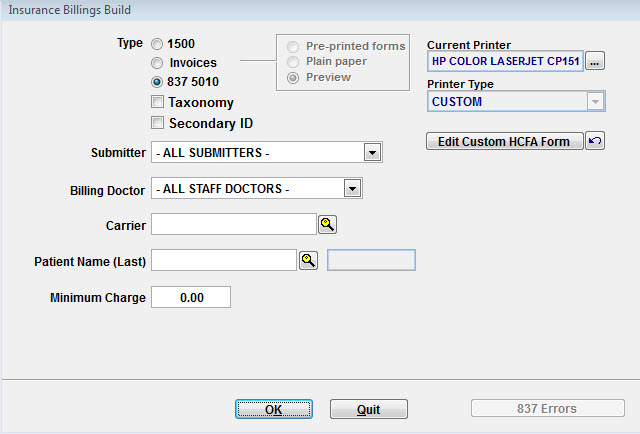
Because ClinicPro encourages electronic billing, the screen defaults to 837 5010. 837 is a billing format for electronic files and 5010 is the version currently being sent. The screen explanation is as follows:
Type
1500 - this option creates HCFA forms. With Clinic Pro, you have the option of choosing preprinted (pink) forms or plain paper. Government payers, i.e. Blue Cross Blue Shield, Medicare and Medicaid require the pink forms. When the payer receives the form, it is scanned by electronic equipment. The pink drops away said that only the black ink is scanned in. Most other payers, commercial payers, allow you to submit claims on plain paper. In this case, Clinic Pro prints all of the boxes and data on regular paper.
Invoices – invoices are used primarily to submit claims to attorneys, employers, or other non-insurance claims. When you set up an invoice system, the name of the payer would be entered into the insurance master file.
837 5010 – this is your electronic billing that will be sent to the clearinghouse.
Taxonomy – in some cases, the insurance carrier wants to receive the taxonomy information in the file or on the HCFA form. If it is required by the insurance carrier, check this box so that the electronic file sends the appropriate information.
Secondary ID – a few insurance carriers are still assigning proprietary IDs to the providers that participate with them. If the insurance carrier requires an ID other than the NPI number, you would check this box.
Submitter – submitters are clearinghouses that will be processing your claims. In order to create an electronic file, you must choose a submitter. To set up your clearinghouse information, click Lists, Submitters. If you are unclear on how to set up the information, please call our support staff.
Billing Doctor – in most cases, you will simply leave this field set to ALL STAFF DOCTORS. ClinicPro automatically separates the billing doctors as it is creating your electronic file. If you have only one Dr. in your practice, you never need to designate billing doctor.
Carrier – if you want to submit claims for a specific insurance carrier, you would use the browse button to choose just that carrier.
Patient Name – you can choose to create files for a specific patient. We sometimes suggest that when a patient has received rejections that have caused an entire file to reject. If you choose to create a file which is that one patient after making necessary corrections, you can send it in alone.
Minimum Charge – if you want to leave out claims that are less than a certain dollar amount, you would fill out the minimum charge. Clinic Pro will automatically ignore those claims while creating a file.
Current Printer – Clinic Pro displays the printer that will be used to print HCFA forms.
Printer Type – this field defaults to Custom since ClinicPro includes the ability to customize your HCFA forms.
Edit custom HCFA form – when you choose this option, you can customize your HCFA form so that it prints in the appropriate lines and boxes for your printer.